The Down and Dirty Side of Electronic Claims
Filing your claims electronically has several advantages. You get your money faster, you don’t have to print claim forms, address envelopes or affix postage.
But then when we started developing software to file electronic claims we quickly realized that just creating claims was not enough.
Claims and the reports received from the clearing house are in Electronic Data Interchange format (EDI). These EDI files are not user friendly and almost impossible to decipher in their raw state without a dedicated reader.
Claim Opened in NotePad
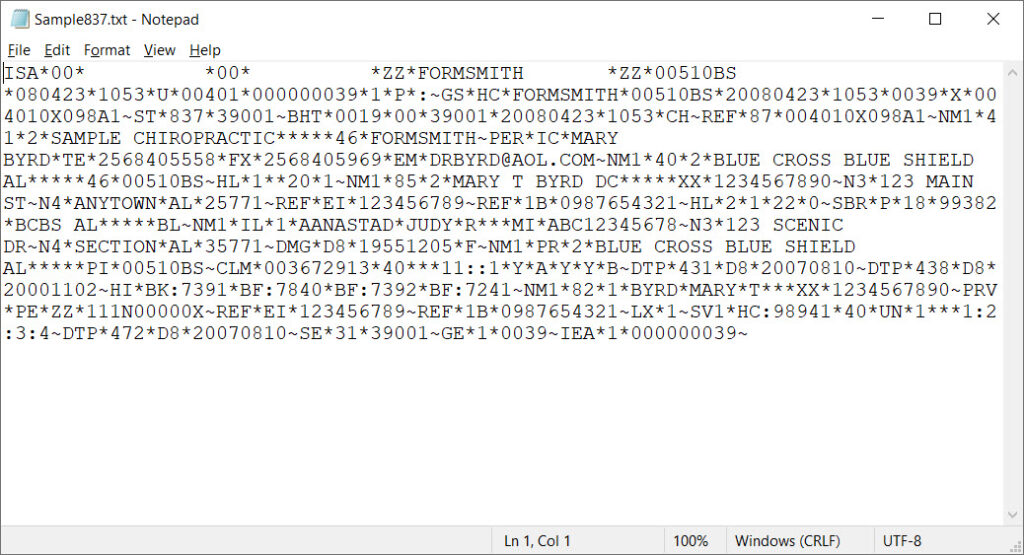
And to make matters even worse, EDI files use codes to report errors and qualify information. Being able to read the file is one thing but to understand the information in it requires access to the codes being used.
Claims have to be uploaded to the clearing house and acknowledgments and remittances have to be downloaded using secure connections (SFTP). This requires specialized software.
Plus sometimes these EDI files are in a ZIP archive and have to be unzipped before they can be used.
Now let’s open the claim file with EDIreader! If the file is zip compressed, EDIreader will unzip the file automatically. When the file is displayed we see:
Claim Opened in EDIreader
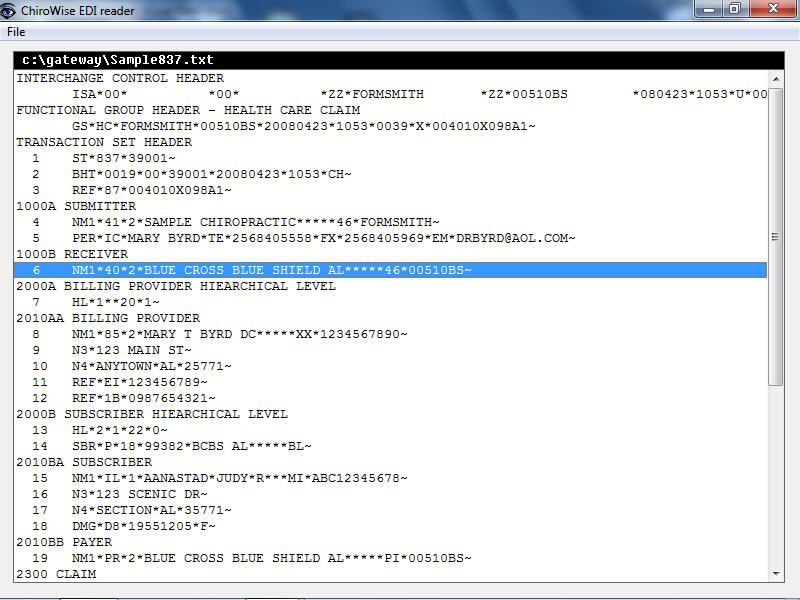
Now It’s easy to find line 6. Also evident is that it is in Loop 1000B – the loop for the receiver information.
Now to isolate the information in error, double-click on line 6 – the NM1 segment. This will break down the segment into its elements:
View NM1 Elements
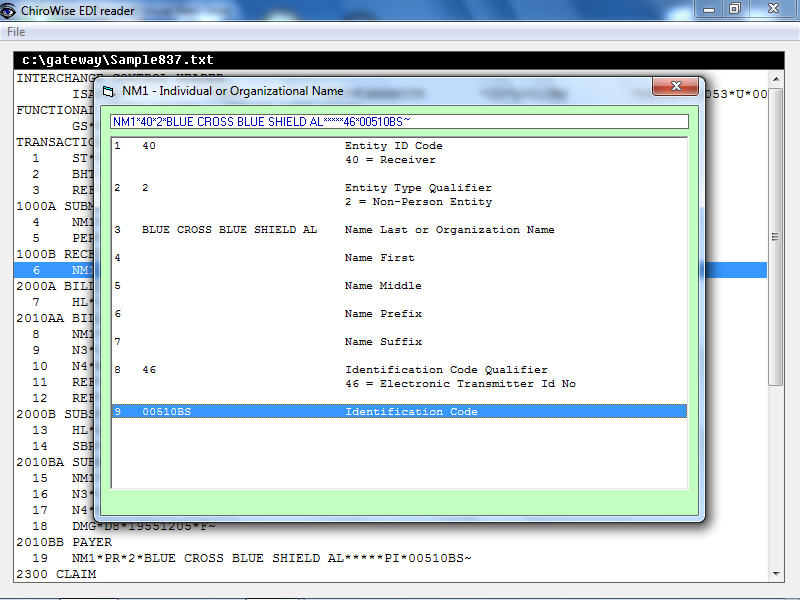
In this case element 9 is the “Identification Code”. The previous element indicates that this code is the “Electronic Transmitter Identification Number.” Conclusion … the insurance company payer ID (00510BS) has been incorrectly entered into your system!
Claim Summary
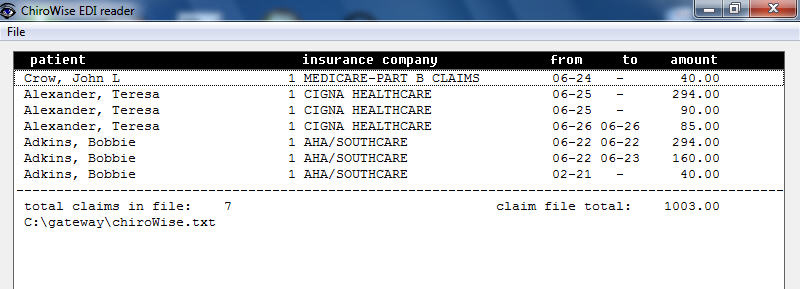
Sometimes it’s helpful to be able to see the claims that are in the claim file. Maybe you want to make sure that a particular patient’s claim is included. EDIreader will show a summary of each patient, their insurance company, the dates of service and the total filed on each claim. And this list can be printed.
Explanation of Benefits
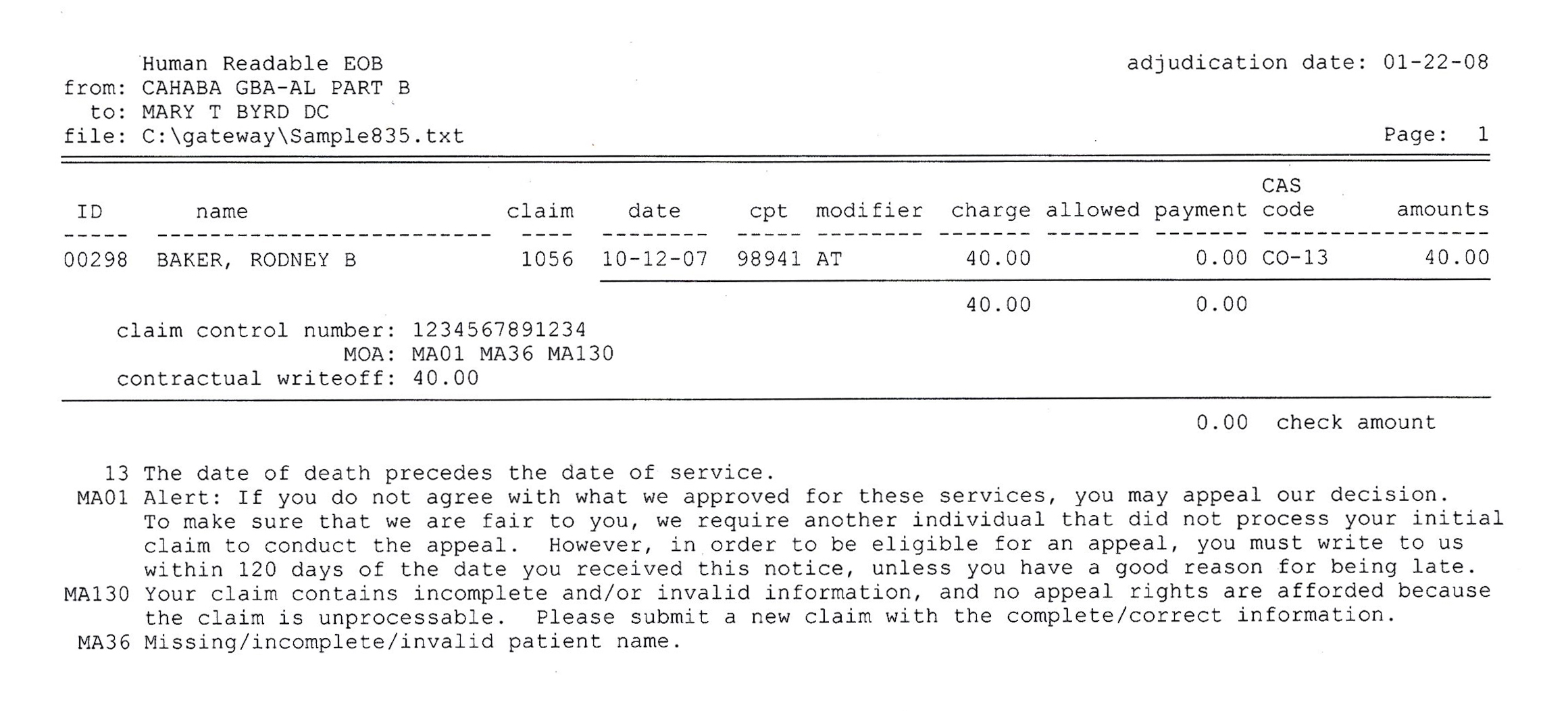
And EDIreader is not just for claims. EDIreader will read the 835 remittance (Explanation of Benefits) which is in EDI format and print a report that looks just like the EOB you get from the insurance company. It includes all the remittance codes that are on the remittance with explanations.
999 Acknowledgement
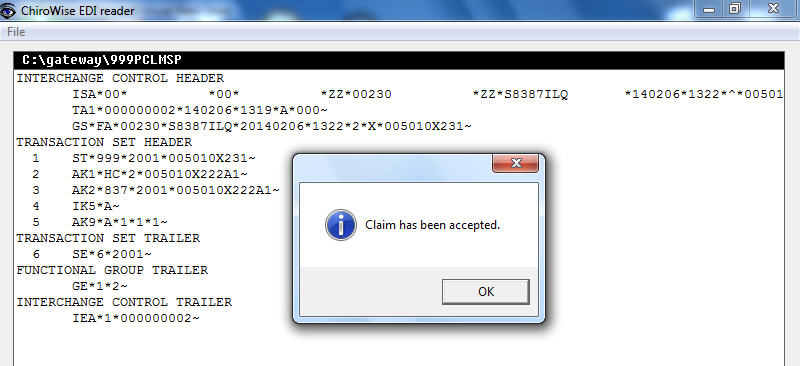
But claims and remittances are not the only files that you may have to deal with. You may also receive a 999 acknowledgment file. This file tells you that the receiver got your file and reports if there were errors in the file.
277 Acknowledgment
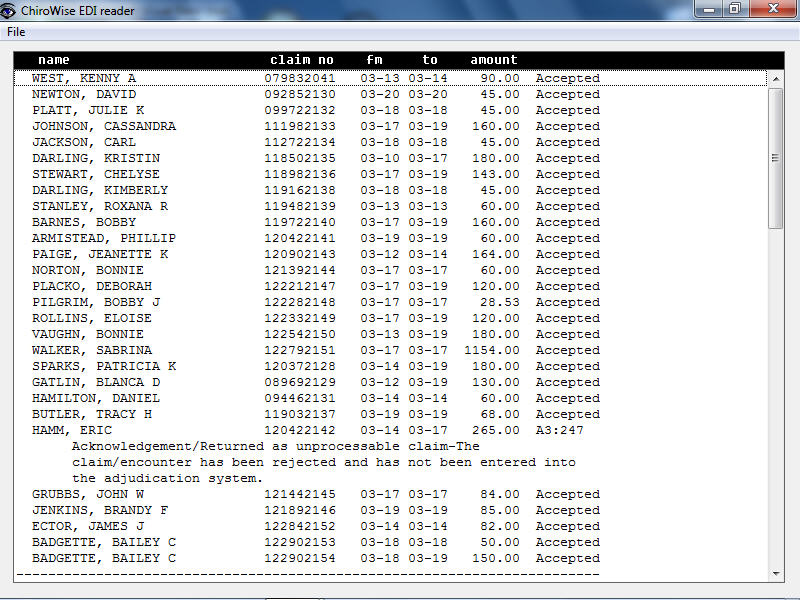
You may also receive a 277 acknowledgement in EDI format. This file will tell you if the individual claims were processable and accepted into the adjudication process. EDIreader produces a human readable report.
What Can EDIreader Do For You?
With EDIreader you will be able to read and understand both the 837 claim that you send to the insurance company or clearing house as well as the 835 remittance that you receive from them. EDI files are not user friendly and almost impossible to decipher in their raw state.
- Zip compressed files do not have to be unzipped in a separate step. They’re automatically unzipped as they are read into EDIreader.
- Loops are Identified – Loops are displayed with both the number (2010A) and the description “BILLING PROVIDER NAME”
- Line numbers are displayed. This is needed when tracking down errors in claims.
- Each segment can be broken down into its elements. Elements are displayed with descriptions.
- A summary of each 837 claim can be printed showing each patient, their insurance company, dates of service and the total filed on each claim.
- EDI reader will read the 835 remittance and print a report that looks just like an EOB received from the insurance company.
- The 999 and 277 EDI acknowledgments can be processed into human readable formats.
- EDIreader has the code sets with descriptions built in so that errors and comments can be shown.
- Included is a claim crosswalk that cross references the HCFA 1500 claim form to the 837 EDI form.
And this is not just software. Included is our basic electronic claims course.
Personal Help Is Available Whenever You Need It
